COVID19 Sudden Cardiac Arrest and Defibrillation
With COVID19 being with us for some time, it is important to prepare for how to manage a Sudden Cardiac Arrest (SCA), Defibrillation and Resuscitation, should it occur.
SCA is indicated when someone becomes unconscious and stops breathing. You will certainly know something is wrong – it will be a drastic event and it will be a lot more alarming than someone having a simple faint or other medical episode such as a stroke, seizure or diabetic hypo (low sugar level)
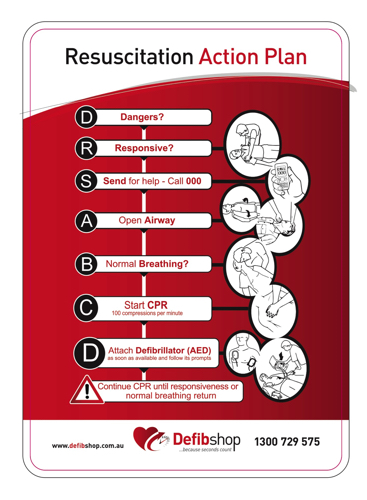
Remember basics first, take a few deep breaths and think about what you need to do. In principle, follow your emergency Resuscitation Action Plan:
D = Dangers
R = Response
S = Send for help – call ‘000’ for paramedics
A = Airway
B = Breathing
C = Compressions
D = Defibrillation
We always need to check for Dangers – danger is all around us no matter what the first aid case is.

With COVID19 invisibly around us anywhere in today’s world, we suggest do not check breathing by putting your face near the patients face. Think of other ways you can assess if the patient is breathing. Here are a few tips…
- Look – look at the patients airway (mouth, neck and chest) to see if you can see any movement that occurs when a person breathes.
- Listen – traditionally, we put our ear down by the patients face to see if we can hear any breathing, or noisy breathing if there is possibly a blockage. However, we suggest not getting this close to the patient with your face during COVID19. And you may still be able to hear breathing from arms length anyway.
- Feel – feeling is a simple way of assessing if a patient is breathing. Feel with the palm of your hand being placed on the patients chest for a few moments, and also on the patients stomach. Our chest is the main area that will move of course as that is where our lungs are housed! However, we can also feel movement at the stomach area too. So feel both areas especially if you are in doubt.
And remember to assess other signs and symptoms too such as the patient’s colour. If you know what their normal colour is, compare their colour now at the time they have fallen ill? Are they pale? Are they going blue or a darker colour than normal around their lips, their ears and fingers?
The above seems like a lot to do and to cover, but you’ll be surprised how quickly you can assess a patient’s condition utilising the above points as you go!
If the patient is UNCONSCIOUS and NOT BREATHING, then immediately begin CHEST COMPRESSIONS (usually referred to as CPR). Current ARC (Australian Resuscitation Council) Guidelines would usually recommend 30 compressions to 2 breaths. However, as we are not doing mouth to mouth now, simply continue with continuous chest compressions – excellent chest compressions – the best you can do, at about 100 to 120 per minute. If you can’t go that fast – then simply do the best you can until help arrives.
Note: Consideration should still be given to giving paediatrics mouth to mouth – especially for instance in a case of drowning.
Don’t forget get your nearest AED (Automated External Defibrillator) / Defib. Remember to always familiarise yourself with where your nearest three defibrillators are located! Being well informed is being well prepared! The earlier you can have an AED on the patient, the quicker it begins to help by talking you all the way through the SCA!
Get others to assist you, and remind all in attendance that we are not doing mouth to mouth as a risk management strategy due to COVID19. Don’t be afraid to summons assistance from family and friends, colleagues, complete strangers and always remember to call ‘000’ to get paramedics on the way to you. If circumstances change in any way, you can call ‘000’ again and update them as required.
As help arrives, if you’ve not had a chance to do it up til then, apply protective equipment. Consider wearing the following if you have it handy:
- Gloves
- Mask
- Glasses or face shield type mask
- Protective gown – if available
Another goodtime to apply your protective gear is whilst you are told to ‘stand clear’ by the AED. You might have time to quickly apply some or all of your protection. And don’t forget, when help arrives, take a break from doing chest compressions and utilise that time to be better prepared with your safety gear!
When the time comes to discard your protective gear, you should where possible dispose of all items in a ‘contaminated waste’ bag. You may also ask the attending paramedics for a contaminated waste bag, and if you have disposed of all your gear prior to the last ambulance leaving, you might ask them nicely if they would take the bag and dispose of it for you properly at the local hospital or their station!
And until the COVID19 climate changes, you could consider attending a COVID19 clinic for testing. Consult your local health and government guidelines to assist you with knowing when you should attend and for a listing of locations to be tested.
Remember, the Defibshop is always here to assist with any questions you may have. Call our number 24/7 for assistance with answers you are looking for. P: 1300 729 575.
Defibshop – makes saving lives easy!
Australia’s No: 1 Defibrillator Store!